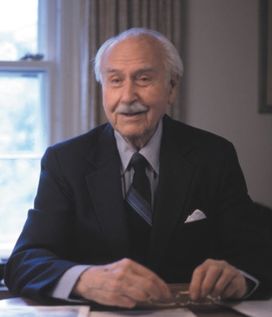
Orvan Hess
- Born
- 1906 June 18
- Baoba, Pennsylvania
- Died
- 2002 Sept. 6
- New Haven, Connecticut
Family
- Father
- Philip Hess
- Mother
- Effie Hess
- Siblings
- Mabel Hess
- Spouse
- Carol Hess
- Children
- Katherine Halloran
Carolyn Westerfield
Known for
- Alma mater
- Lafayette College
University at Buffalo - Fields
- Obstetrics
Gynecology - Institutions
- Yale New Haven Hospital
Yale School of Medicine - Awards
- AMA Scientific Achievement
Orvan “Bop” Walter Hess, M.D. (1906 June 18 – 2002 Sept. 6), husband of Carol Maurer Hess, father of Kitty Halloran and Carolyn Westerfield.
Contents
AMA Scientific Achievement Award
- See also “A clinician’s research feats” (27 July 1979) American Medical News.
The 1979 Scientific Achievement Award has been granted to Doctor Orvan W. Hess from the Yale University School of Medicine in New Haven, Connecticut.
Doctor Hess is an obstetrician/gynecologist who is being honored for his development of procedures and equipment to accurately monitor the fetal heartbeat. He began his work in this area around 1937 when he was still a resident. In 1957, for the first time, it became possible to isolate the fetal heart rate from the mother's during labor and determine whether changes in rate and rhythm were related to uterine contractions or abnormal obstetrical conditions. Doctor Hess has continued his research in this area and during the 1960s devised a system of telemetering the fetal electrocardiogram and intrauterine pressure during pregnancy and labor. Thus it is possible to keep a continuous, accurate check on the unborn baby's heartbeat even when medical personnel are unable to be right in the same room. The electrical signals are monitored and transmitted by short-wave radio signals. Further refinements include reducing the equipment in weight and size making it easier to use and more adaptable during many types of operations on pregnant women, and using ultra-sound to monitor the fetal heart activity continuously from the external abdominal wall of the mother. The results of his work have been widely published and he has lectured on the subject throughout the United States and numerous countries around the world.
He has served as the President of the Connecticut State Medical Society, as the Medical Director of the state Welfare Department, and is currently an AMA Delegate.
He received his M.D. Degree from the University of New York at Buffalo in 1931. He is a member of the American College of Obstetricians/Gynecologists and American College of Surgeons.
The Scientific Achievement Award is made only on special occasions and presented at the AMA Annual Meeting before the House of Delegates. It comes in the form of a medallion and a $ 2,500 stipend given to a physician or non-physician selected by the Board of Trustees in recognition of outstanding work.
Members of the board of trustees, officers, fellow members of House of Delegates and guests:
It is with great appreciation that I accept this award of the A M A personally and in behalf of my many colleagues—some of whom are here today—who have contributed so much to the development and use of electronic techniques of monitoring the fetus. I wish to pay particular tribute to Drs. Ed Hon, Ted Quilligan and Dick Paul, full-time investigators, and to Dr. Kubli of Heidelberg, and Dr. Takemura of Tokyo who were involved in early studies at Yale. Also, I wish to express my appreciation to my many private patients and their unborn fetuses whose voluntary participation was essential to our investigations.
I have been comfortable with the principles of the AMA which respect the freedom of the individual doctor to practice. Now I find after all these years that I am held accountable for my behavior!!
It is my impression that in conferring this award you are in effect recognizing an idea.
It has been said that ideas are the result of partly intuition and partly reason.
Exposed to the rich heritage of obstetrical accomplishments at Yale and surrounded by full-time educators and inspiring clinicians, bio-chemists, electrical engineers, and even economists—I could not escape at least one creative impulse!
In this case, I was motivated by a perceived need to find a better way of determining those fetuses in distress. Intuition directed me to observe the fetal heart action and reason led me to use electrical devices.
Ideas may be classified in at least two categories: 1) those that border on science-fiction and 2) perhaps most important, those which are “fundable”. When I expressed the desire to determine fetal heart activity by means of electrocardiography, I was fortunate to have it considered “fundable”. When I received financial support of $700 from the United Way and $1,065 from the New Haven Heart Association, I was elated, although it was a paltry sum by present standards. Later, I received a substantial gift from my patient, Mrs. Frederick Hilles, who made it possible for me, in collaboration with Dr. Hon, a Markle Research Fellow at the time, to continue the development of electronic apparatus necessary for continuous recording of F.H.R. and uterine activity. More recently, the Theodore Barth Foundation has supported my research on radio-telemetry and ultrasound.
The innovative approach of electronic monitoring was in line with the applications of technology which helped advance medical diagnosis and therapy rapidly in the ’50s and resulted in extending human longevity.
Through improvements in perinatal care and technological advances including fetal monitoring, the perinatal mortality rate has been reduced by 50 percent in the United States during the past two decades.
This has meant that literally thousands of persons are alive and contributing to the welfare of society—persons who might not otherwise be alive if the technology had not been achieved.
From my personal observations in several countries—including India, Japan, England and West Germany, I am convinced that we have available in the U.S. the highest quality medical care in the world. To a large extent, this is a reflection of the advances in technology.
The point of view, held by some pessimists (medical nihilists, if you will) who would return to a past era of “watchful waiting” in obstetrical management, and when decisions were often made on inaccurate data, seems completely unacceptable to me.
I feel we have been somewhat remiss in not moving more rapidly to incorporate teaching programs in the curricula of our institutions of education for doctors, nurses and allied health personnel, to promote understanding and maximum benefit of technology.
The medical profession is about to experience the impact of the new Federal Center of Technology Assessment and other regulatory bodies which have been established to evaluate safety, efficiency and cost. The AMA is committed to cost-containment. While we recognize the importance of these evaluations it is hoped that not too much emphasis will be placed on cost-benefit analysis and that they will not impede the progress of innovation in medical technology.
Innovative technology comes about in many ways. For example, I am reminded of the late Gordon Maurer, who was a fine surgeon, a strong advocate of research and a humanist. After graduating at the top of his class from both the Yale Scientific School and the Yale Medical School, and completing his training in surgery, he had many excellent offers. Instead, he chose to practice in Margaretville, a small village in the Catskill Mountains in upper New York State, while still maintaining ties with the medical school and continuing his research.
It was my good fortune while a student on vacations from college and medical school, to accompany this family physician on home visits, assist him with surgery (including cesarean sections), often done on a kitchen table, and with his research on intestinal anastomosis, this stimulating experience greatly influenced my life.
Excerpts from an editorial in the Catskill Mountain News which express the community’s reaction to his untimely death:
- …there came here a city chap, trained in one of the great universities.
- Soon after arrival he was called upon to care for a life given up as lost. He saved it.
- He began to save others, he worked day and night.
- When he did not have proper apparatus or appliances he built some.
- When the snows kept him from patients he constructed a snowmobile.
- He was physician, parson, priest, confessor—we told him both our physical and mental troubles and he put us back on the road to reason and living.
- Today our hearts are numb at his loss, our senses befogged to know how to live without him.
- …thank god for those thirteen years.
I believe these sentiments are symbolic of my belief that technology can be applied to practice without sacrificing humanism or our sacred patient-physician relationship.
I am pleased to tell you that Dr. Maurer’s sister, Carol, my wife, is here today. ― Orvan W. Hess, M.D.,
Obituaries
New York Times
Dr. Orvan W. Hess, Who Developed Fetal Heart Monitor, Dies at 96
Dr. Orvan W. Hess, an obstetrician and gynecologist who pioneered the development of the fetal heart monitor and was instrumental in the first successful clinical use of penicillin, died on Sept. 6 at Yale-New Haven Hospital. He was 96.
The fetal heart monitor has been credited with reducing the number of stillbirths and with helping hospitals run more efficiently, because it allows nurses to monitor more than one patient at a time.
“Other than ultrasound, it is probably the most widely used technique in all of obstetrics,” said Dr. Joshua Copel, a professor of obstetrics, gynecology and pediatrics at the Yale University School of Medicine. But in recent years, Dr. Copel noted, there has been debate about whether continuous monitoring of fetal heartbeat in labor has led to an unnecessary increase in Caesarean sections.
The idea for the fetal heart monitor sprang from Dr. Hess’s early frustration with what he called the “watch and wait and pray” method of childbirth, in which the doctor had no way to determine if the fetus was in distress. The only tool doctors had to detect the heartbeat of a fetus was a stethoscope, but it also picked up the heartbeat of the mother, and when the mother was having contractions—the time of most stress for the fetus—it was impossible to detect a fetal heartbeat.
“Before these monitors were invented, the uterus was literally a black box,” Dr. Copel said. “We knew the babies were in there, and they came out.”
Dr. Hess began work on a way to electronically measure fetal heart activity in the 1930’s when he was a resident in New Haven and a research fellow at the Yale medical school. His work was interrupted by World War II service as a surgeon in the front-line hospital attached to Gen. George S. Patton’s Second Armored Division in the invasions of North Africa, Sicily and Normandy.
When Dr. Hess returned to Yale in 1949, he resumed his work, along with Dr. Edward Hon, a postdoctoral fellow. In 1957, using a six-and-a-half-foot-tall machine, they became the first in the world to continuously detect and record fetal electrical cardiac signals.
In the 1960’s, working with Wasil Kitvenko, the chief of the medical school’s electronics laboratory, Dr. Hess continued to improve on the equipment, introducing telemetry and reducing the monitor’s size.
This was not Dr. Hess’s first involvement in a pioneering medical moment. In 1942, one of his obstetrics patients contracted scarlet fever, which caused a miscarriage and subsequent streptococcus infection.
“Doctors had done everything possible, both surgically and medically,” Dr. Hess said in a 1998 interview with Katie Krauss, the editor of Yale-New Haven Magazine and one of the many babies Dr. Hess delivered. “I went to see her and knew she was dying.”
Dr. Hess wanted to talk to her internist, Dr. John Bumstead, and found him asleep in the library. “While I was waiting for him to wake up,” Dr. Hess said, “I sat and read the latest Reader’s Digest, in which there was an article called “Germ Killers From Earth,” about the use of soil bacteria to kill streptococcal infection in animals.”
He asked Dr. Bumstead, “Wouldn't it be wonderful if we had something like this gramicidin mentioned in the Reader’s Digest?” This prompted Dr. Bumstead to speak with some colleagues who were studying penicillin and to obtain some for the patient, Anne Miller. The day after her first injection, Mrs. Miller’s fever broke. She lived to be 90 years old, dying in 1999.
A few months later in St. Louis, where doctors were discussing streptococcal septicemia, Dr. Hess stood to tell of the success with penicillin.
“They listened politely,” Dr. Hess recalled, “and then the moderator said, “That’s fine, son, now you continue with your studies—and keep us informed.” He just brushed my comments aside.”
Orvan Walter Hess was born on June 18, 1906, in Baoba, Pennsylvania. Two years later—after his mothers death—the family moved to Arena, New York, and soon thereafter to the farming community of Margaretville, N.Y.
When he was in high school a graduate of the Yale medical school who had moved to the community to found a hospital encouraged him to attend college and become a doctor.
He graduated from Lafayette College in 1927, then earned his medical degree from the University of Buffalo. After an internship at Children’s Hospital in Buffalo, Dr. Hess moved to New Haven, where he had a residency at New Haven Hospital and then became a fellow and clinical instructor at Yale.
In 1979, he received an American Medical Association scientific achievement award for his contributions to clinical research. He was president of the Connecticut State Medical Society and was director of health services for the Connecticut Welfare Department in the early days of Medicaid and Medicare.
His wife, the former Carol Maurer, died in 1998. He is survived by two daughters, Dr. Katherine Halloran of Lexington, Mass., and Carolyn Westerfield of Hamden, Conn.; five grandchildren; and five great-grandchildren. ―
Yale Daily News
Orvan Hess, inventor of fetal heart monitor, dies at age 96
Dr. Orvan W. Hess, a fellow at the Yale School of Medicine who developed the fetal heart monitor, died on Sept. 6 at Yale-New Haven Hospital. He was 96.
Hess, an obstetrician and gynecologist, was also a pioneer in the clinical use of penicillin to treat bacterial infections.
The fetal heart monitor, which is used to detect early signs of fetal distress during labor, has been credited with reducing the number of stillbirths.
“It was a huge change because it allowed us to get an initial understanding of what was going on for the fetus during labor,” said Dr. Joshua Copel, a professor of obstetrics, gynecology and pediatrics at the medical school.
While developed for “high-risk” pregnancies, fetal monitoring is also applied in the majority of normal pregnancies.
“It’s a ubiquitous tool in obstetrics,” Copel said.
It was while Hess was a research fellow at the medical school in the 1930s that he began his work on a way to electronically measure fetal heart activity. After serving in World War II as a surgeon, Hess returned to Yale in 1949 and continued his work alongside Dr. Edward Hon.
Hess received the American Medical Association’s scientific achievement award in 1979 for being one of the first doctors to report the successful use of penicillin as a treatment for a streptococcus infection.
He served as president of the Connecticut State Medical Society and director of health services for the Connecticut Welfare Department.
Hess’ wife died in 1998. He is survived by two daughters, five grandchildren and five great-grandchildren. ―
the Lancet
Orvan Hess
Obstetrician and gynaecologist who developed the fetal heart monitor; first to use penicillin in USA; faculty member at Yale University School of Medicine; advisor to a US President. Born June 18, 1906, in Baoba, Pennsylvania, USA; died after a brief illness aged 96 years on Sept 5, 2002.
Orvan Walter Hess was, in the words of one prominent colleague, an “enthusiastic and energetic” obstetrician, gynaecologist, and World War II surgeon who pioneered fetal-heart-rate monitoring and was the first to use penicillin in the USA, in a patient with scarlet fever.
Hess is perhaps best known for his work, which he started as a young faculty member at Yale in the late 1930s, on ways to monitor the fetal heart rate. Although a colleague, Edward Hon, is often regarded as the father of the technique, Hon only became interested in such research some 10 years after Hess, according to a letter from Hon found by Joshua Copel, professor of obstetrics and gynaecology and head of maternal-fetal medicine at Yale. Hess and Hon’s work resulted in a 1957 paper in Science in which they described the first equipment to record the fetal heart rate—more than 6 feet tall and 2 feet wide. The work continued after that, as the team, along with Wasil Kitvenko, head of Yale’s electronics laboratory, refined the device. Today, of course, such equipment is much smaller and its use has substantially reduced the number of stillbirths—although, somewhat predictably, it is also argued that the fetal heart monitor has increased the number of unnecessary caesarian sections.
The story of Hess’ use of penicillin in 1942 is one of serendipity and courage. When a patient, Anne Miller, developed scarlet fever and streptococcal septicaemia, Hess went to speak to Miller’s internist, John Bumstead, finding him asleep in the library. Hess happened on an article in Reader’s Digest on the use of soil bacteria to kill streptococcus in animals. According to a 1988 article in the Chicago Tribune Magazine, Hess and Bumstead convinced government officials to give them some 5.5 g of penicillin—about half the available supply of the drug in the USA. At that time, penicillin had only been tried, unsuccessfully, in one patient in the UK. They administered it to Miller, whose fever broke within 24 h and who lived to the age of 90 years.
Although less well-known, Hess made other important and wide-ranging contributions to medical science. His first paper, in 1936, described the use of cat gut in the perineum. He also published works on vascular injuries of the extremities in casualties of war.
Hess, who grew up in a farming community, graduated from Lafayette College, Easton, PA, in 1927 and received his medical degree from the University of Buffalo, New York, in 1931. He went on to serve his internship in orthopaedics and surgery at the Children's Hospital of Buffalo, followed by a year in surgery, gynaecology, and obstetrics at Yale-New Haven Hospital, and a residency in obstetrics and gynaecology that he completed in 1937.
Apart from his service during World War II in the 91st Evacuation Hospital of the US Army, where he served under General George S. Patton in North Africa, Sicily, and Normandy, Hess worked at Yale in research and on the wards delivering children for his entire career. He retired from Yale’s faculty in 1975, but remained “a visible member of the staff”, according to Copel. In 1979, he received an American Medical Association scientific achievement award. Hess, who was certified by the American Board of Obstetrics and Gynecology and by the American College of Surgeons, also served as president of the Connecticut State Medical Society and on many state and national policy-making committees, including President Lyndon B Johnson's White House Conference on Medicare.
Hess is survived by two daughters, five grandchildren, and five great-grandchildren. His wife died in 1998.
Charles Lockwood, now the chairman of obstetrics and gynaecology at Yale, said he received a note from Hess just this August congratulating him on his appointment. “He signed his note with a crisp, clear signature”, Lockwood recalls, “I suspect he retained his enthusiasm to the end”. ―
Yale Bulletin & Calendar
Dr. Orvan Hess, who helped develop fetal heart monitor, dies at 96
A memorial service will be held on Wednesday, Dec. 4, for Dr. Orvan W. Hess, clinical professor emeritus of obstetrics and gynecology and a fellow of Morse College, who died Sept. 6 at the age of 96 after a short illness.
The service will be held at 11 a.m. at Spring Glen Church, corner of Whitney Avenue and Glendower Road in Hamden. A reception will follow the service.
Dr. Hess pioneered the development of the fetal heart monitor and was instrumental in the first successful clinical use of penicillin in the early 1940s.
A native of Margaretville, New York, Dr. Hess came to Yale-New Haven Hospital in the 1930s after completing his undergraduate degree at Lafayette College, his M.D. at the University of Buffalo and an internship at Children's Hospital in Buffalo, New York. Also a research fellow at the School of Medicine, he began work on a way to measure fetal heart activity. His work was interrupted by World War II, when Dr. Hess served as a surgeon in the front-line hospital attached to General George S. Patton's Second Armored Division in the invasions of North Africa, Sicily and Normandy.
After the war, Dr. Hess returned to Yale and continued his work developing a fetal monitor. The first, a six-and-one-half-foot-tall machine, was introduced in 1957. Dr. Hess and a Yale colleague were the first to detect and record electrical cardiac signals. Throughout the 1960s, Dr. Hess continued to improve his design of the machine, making it smaller and introducing telemetry.
“Other than ultrasound, it is probably the most widely used technique in all of obstetrics,” said Dr. Joshua Copel, a Yale professor of obstetrics, gynecology and pediatrics, in The New York Times obituary for Dr. Hess. “Before these monitors were invented, the uterus was literally a black box. We knew the babies were in there, and they came out.”
In 1942, Dr. Hess helped save a dying obstetrics patient who had scarlet fever. He mentioned to the woman's internist an article he read about the use of certain antibiotics to kill infections in animals. This prompted the internist to consult with some colleagues who were studying penicillin and to obtain some for the patient. The woman went on to live until she was 90 years old.
For his work, Dr. Hess was honored with the Scientific Achievement Award from the American Medical Association. He was president of the Connecticut State Medical Society and served as director of health services for the Connecticut Welfare Department in the early days of Medicaid and Medicare.
Dr. Hess was predeceased by his wife, the former Carol Maurer, who died in 1998. He is survived by two daughters, Dr. Katherine Halloran of Lexington, Massachusetts, and Carolyn Westerfield (Mrs. H. Bradford Westerfield) of Hamden; five grandchildren; and five great-granddaughters. ―
Encyclopædia Britannica
Orvan Walter Hess
American obstetrician and gynecologist (b. June 18, 1906, Margaretville, N.Y.—d. Sept. 6, 2002, New Haven, Conn.), developed the first fetal heart monitor, at the Yale University Medical School, in 1957. The device, which allowed monitoring to continue during labour, became, except for ultrasound, the most-used technique in obstetrics. Hess also played a major part in the initial successful employment of penicillin clinically, when in 1942 he saved the life of an obstetrical patient suffering from a streptococcal infection. ―
A Catskill Catalog
Orvan Walter Hess
Orvan W. Hess grew up in Margaretville. His family moved up here in 1908 from Pike County, Pennsylvania, downriver on the Delaware. It wasn’t a happy move: little Orvan’s mother had just died. I would guess she died trying to give birth to another child. Maybe that’s why Orvan became an obstetrician.
Lots of women died in childbirth in the first years of the 20th century. My maternal grandmother died before she turned 30, trying to bear a stillborn son.
Visits to early cemeteries often reveal a series of wives per husband, with tragically early death too common among young women.
Dr. Orvan W. Hess was a major contributor to the advancement of obstetrics and gynecology as branches of scientific medicine. He pioneered the use of penicillin. He invented the fetal heart monitor. He was a clinical professor at Yale School of Medicine. He was a Catskill Mountain kid.
The Hess house was on Orchard Street in Margaretville, a stately white clapboard Victorian that sits elegantly on a gentle rise above the street. Behind it is a barn, a stable actually, a proper Victorian village livery. One summer, years ago, I painted it, along with a partner. Dr. Hess’s sister lived there then, although, I think, by that time, the house was mostly used summers.
Little Orvan attended the village school, a short walk from his home. The grades were organized two to a classroom, up to grade eight. Orvan was smart, a good student. Perhaps, he skipped a grade or two. By early adolescence, Orvan entered the Academic Department of Margaretville High School. The Margaretville Firehall now occupies that old school building.
Margaretville High School attracted the best students from the Town of Middletown’s 26 common schools, mostly one-room rural schools that served an area in a valley, hamlet, or hollow no bigger than five square miles. Students from as close as New Kingston often boarded in Margaretville to attend school.
Going to high school was a big thing. Graduating, even bigger. Most kids left school after eighth-grade.
Orvan Hess was an honor student, interested in the sciences. He fell under the sway of Dr. Gordon Bostwick Mauer, the young Yale grad who had come to Margaretville to practice hands-on rural medicine, who started the Margaretville Hospital in his own house.
The presence of Dr. Maurer’s sister, Carol, was another reason young Orvan had to hang out at Dr. Maurer’s. Carol Maurer became Orvan Hess’s wife of 70 years. They married in 1928, a year after Orvan graduated from Lafayette College in Easton, Pennsylvania, a school Dr. Maurer had urged him to attend.
From Lafayette, Orvan went to medical school at the University of Buffalo. After an internship at Buffalo’s Children’s Hospital, Dr. Hess accepted a residency at New Haven Hospital. Soon, he was a fellow and clinical instructor at Yale.
In 1942, Dr. Hess participated in the first successful clinical use of penicillin. A patient, Anne Miller, was clearly dying. “Doctors had done everything possible, both surgically and medically,” Dr. Hess told a 1998 interviewer for Yale-New Haven Magazine. The obstetrician-gynecologist went to confer with the patient’s internist, Dr. John Bumstead.
Dr. Bumstead was asleep in the medical library. I guess professional courtesy precluded waking up the sleepy internist, so Dr. Hess sat and waited. He described to his interviewer his eureka moment.
“While I was waiting for him to wake up, I sat and read the latest Reader’s Digest, in which there was an article called ‘Germ Killers From Earth,’ about the use of soil bacteria to kill streptococcal infection in animals. Wouldn’t it be wonderful if we had something like this gramicidin mentioned in the Reader’s Digest?”
Dr. Hess’s suggestion led Dr. Bumstead to procure some penicillin from researchers nearby. They gave Mrs. Miller a shot, and, the next day, her fever broke. Anne Miller lived to be 90!
In 1979, Dr. Orvan Hess received the “Scientific Achievement Award” from the American Medical Association for this breakthrough medical moment.
Dr. Hess’s greatest achievement, however, was the development of the fetal heart monitor. He began tinkering on it in the 1930s, frustrated by the confusion and clinical inaccuracy of stethoscopes trying to monitor two different heart beats during labor contractions. This three-sound welter of pulses made it extremely difficult to identify a fetus in distress until it was too late.
By 1957, he and Dr. Edward Hon had built a six-foot contraption that was the first machine to measure, continuously, the electrical signals produced by the fetal heartbeat. Use of the fetal heart monitor soon became standard obstetrical procedure.
Dr. Hess continued, for many years, to practice in New Haven and teach at Yale, while maintaining the family’s Catskill Mountain home in Margaretville. He died in September 2002, one of the most celebrated medical practitioners of the 20th Century, a Catskill Mountain kid. ―
References
- ↑ Baranauckas, Carla (September 16, 2002) “Dr. Orvan W. Hess, Who Developed Fetal Heart Monitor, Dies at 96” The New York Times.
- ↑ Dervan, Andrew (September 18, 2002) “Orvan Hess, inventor of fetal heart monitor, dies at age 96” The Yale Daily News. Yale University.
- ↑ Oransky, Ivan (12 October 2002) “Orvan Hess” The Lancet, Vol. 360, p. 1179.
- ↑ Yale University (November 22, 2002) “Dr. Orvan Hess, who helped develop fetal heart monitor, dies at 96” Yale Bulletin & Calendar, Vol. 31, No. 12.
- ↑ Sparks, Karen (December 31, 2002) “Orvan Walter Hess” Britannica Book of the Year 2003. Encyclopædia Britannica. ISBN 978-0852299562.
- ↑ Birns, Bill (June 9, 2010) “A Catskill Catalog” Catskill Mountain News.